Fluvoxamine in the treatment of binge-eating disorder
Continued "Since the s, people have recognized that the same substances that control mood also control appetite.
If there's a low level of serotonin, one may feel depressed but also crave high-carbohydrate, binge-type foods. Consuming high-carbohydrate foods results in increased production of brain serotonin. Thus, the body may be self-medicating by bingeing.
Equal numbers of patients were scheduled to be randomly assigned to receive either drug or placebo. All medications were in identical capsules 50 mg of fluvoxamine or placebo supplied in numbered containers dispensed to patients according to the randomization schedule.
During the placebo lead-in period, patients took one capsule each evening; once a patient entered the double-blind treatment phase, the dose was 50 mg each evening for a minimum of 3 days. Beginning on day 4, the dose could be adjusted on an individual basis between 50 mg and mg until the end of week 9. If the number of capsules was even, an equal number of capsules was taken in the morning and evening; if the number of capsules was odd, the greater number of capsules was taken in the evening.
Adjustments within the range of one to six capsules per day were at the discretion of the investigator, and medication was increased within this range until a patient was asymptomatic or intolerance intervened.
In addition, these subjects had reported at their screening visit a history of at least three binge-eating episodes per week for at least 6 months as opposed to an average of only two episodes per week, as required in the draft criteria. It should be noted that the only change from the draft criteria to those ultimately adopted in DSM-IV was the requirement that the binge eating occur, on average, at least 2 days a week for 6 months.
All of the patients reported on here would have met the criterion of 2 days per week as well as that of three episodes per week. For screening purposes and throughout the course of the study, we defined a binge by using the DSM-IV criteria plus the additional requirement that the estimated number of calories consumed be at least kcal. Patients were disqualified if they were pregnant or lactating; displayed concurrent anorexia nervosa, concurrent or recent within 1 year of study entry major depression or obsessive-compulsive disorder or lifetime substance dependence, psychosis, mania, or organic dementia; posed a significant suicide risk; had received psychotherapy or behavioral therapy within 3 months of entry to the study; had a history of psychosurgery or seizures; had a history of any psychiatric disorder that could interfere with diagnostic assessment, treatment, or compliance; had clinically unstable medical illness; had clinically significant abnormal laboratory results; had received monoamine oxidase inhibitors MAOIs , tricyclics, neuroleptics, lithium, or fluoxetine within 4 weeks before randomization; had received investigational medications or depot neuroleptics within 3 months before randomization; had previously received fluvoxamine; or had fewer than three binges in the week before randomization i.
Procedures Patients were seen weekly during the study. At the first visit, the following were obtained, ascertained, or performed: Patients were given diaries at this and each of the following visits in which to record any binges and, once medication was initiated, the number of capsules of medication taken. At each subsequent visit, patients were assessed for number of binges experienced since the last visit, medication dose, medication compliance through capsule count, any adverse events, any nonstudy medications, and vital signs.
The item Hamilton Depression Rating Scale 18 was administered at the baseline, week 5, and week 9 visits. Secondary outcome measures were Hamilton depression scale scores, body mass index, and response categories. We also assessed the following safety measures: Statistical Methods Prestudy comparisons were made by using the following variables at randomization: For the analysis of each outcome measure except response category , we used the computer program SAS PROC MIXED 19 to perform a repeated measures random regression analysis comparing the rate of change of the measure in the fluvoxamine-treated group compared with the placebo group see Gibbons et al.
We began with a model for the mean that included terms for treatment, time, center, treatment-by-time interaction, and treatment-by-center interaction. We used the logarithmic transformation because the response of the outcome measures was approximately linear on the log scale, as is often found in treatment studies in psychiatric disorders For testing, we first checked for a significant treatment-by-center interaction. This interaction was found to be nonsignificant on all measures; therefore, we dropped terms for this interaction from the model.
We retained the terms for effects of center in all analyses, regardless of whether the effect of center was significant. The term of interest was the treatment-by-time interaction, which can be interpreted as the difference in the rate of change change per unit of time , or the difference in slope with respect to time, of the outcome measure.
We initially modeled the covariance of observations on the same individuals as having a heterogeneous first-order autoregressive structure. Specific forms of psychotherapy, or talk therapy—including a family-based therapy called the Maudsley approach and cognitive behavioral approaches—have been shown to be useful for treating specific eating disorders.
Evidence also suggests that antidepressant medications approved by the U. Food and Drug Administration may help for bulimia nervosa and also may be effective for treating co-occurring anxiety or depression for other eating disorders.
Treatment plans often are tailored to individual needs and may include one or more of the following: Individual, group, or family psychotherapy Medical care and monitoring Nutritional counseling Medications for example, antidepressants.
Some patients also may need to be hospitalized to treat problems caused by malnutrition or to ensure they eat enough if they are very underweight. Complete recovery is possible. What is being done to better understand and treat eating disorders?
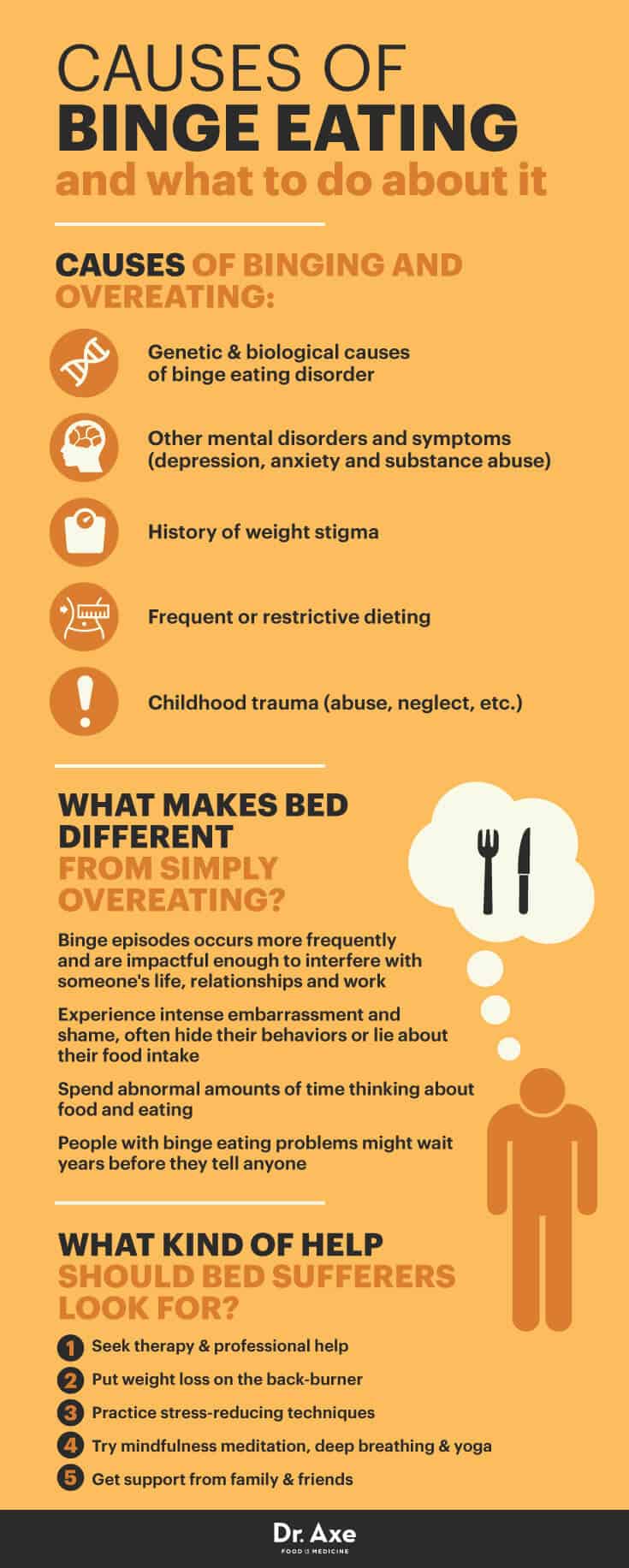
Researchers are finding that eating disorders are caused by a complex interaction of genetic, biological, psychological, and social factors.
Little is known about the family characteristics of BED patients. One study found that BED subjects rated their family environment as less supportive and cohesive, and less engendering of direct and open expression of feelings than healthy controls. The BED group scored worse than other eating disorder groups. Obesity is found to develop several years after the onset of binge eating. The central criterion for BED is the occurrence of episodes of binge eating which is also an essential criterion for bulimia nervosa.
Obesity with and without binge eating disorder Obese patients with BED have less self-esteem and greater depressive symtomatology than obese persons without BED; they also have more comorbid psychiatric disorders, in particular affective disorders and personality disorders. There is even a tendency for underreporting weight. Two studies have recorded food intake in a laboratory. Also, the recorded energy intake of subjects with BED on non-binge days was greater than that recorded by subjects without the disorder.
Subjects with BED consumed more dessert and more snack foods more fat and less protein than did obese control subjects. The total intake was larger and duration of the episodes was longer in subjects with BED.
Furthermore, for both subjects with and without BED, it seems that energy intake increases with the degree of obesity. Purging bulimics engage in self-induced vomiting, misuse of laxatives, diuretics or enemas to compensate for binge eating. Non-purging bulimics use inappropriate compensatory behaviours like fasting or excessive exercise. Several studies have compared BED patients with purging bulimics, 31 , 47 , 52 , 53 , 54 , 55 , 56 , 57 , 58 and a few studies have compared BED patients to non-purging BN patients.
Compared to subjects with BN DSM-III-R subjects with BED seem less anxious about their eating patterns and bodyweight, feel less guilty about being overweight, are less preoccupied with their eating behaviour, have a better overall opinion of themselves, are able to perceive internal states more accurately, are more socially adjusted, and are more comfortable in maintaining interpersonal relationships.
Non-purging bulimics and BED subjects do not seem to differ in clinical and psychological characteristics, such as psychiatric symptoms, frequency of bingeing, and impulsiveness traits. However, on many of the variables, the BED group showed a significantly greater variance. In a laboratory subjects were asked to binge on ice cream.
No difference was observed in the mean number of consumed calories. Studies which compared BED, BN and obesity 32 , 53 , 54 indicate that individuals with BED exhibited levels of psychopathology that fell somewhere between the high levels reported by individuals with BN and the low levels reported by obese individuals without binge eating. However, the characteristics of subjects with BED seemed to bear a closer resemblance to those of subjects with BN than to those of obese individuals.
It has also been suggested that BEDs exist on a continuum of clinical severity, which starts with BN purging type most severe , passes through BN non-purging type intermediate severity , and finishes with BED least severe. The operationalization of the binge eating criteria in BED poses several problems see Table 1. By comparison, episodes of binge eating are easier to define in BN because the binge eating is followed by compensatory behaviour like vomiting.
In BED both the beginning and ending of an episode of binge eating are less clear. Also, there is no consensus about the best method for assessing binge behaviour, ie is it better to count the number of binge days or the number of binge episodes. This is also reflected in the discrepancy between criterion A1 and D. Since research changes so quickly, some or all of the information listed on this page could be out of date.
Please use the following information as a guide only and a starting point from which to do further research. A good research tool is www. Medication can't cure an eating disorder. However, medications may help you control urges to binge or purge or to manage excessive preoccupations with food and diet.
Medications such as antidepressants and anti-anxiety medications may also help with symptoms of depression or anxiety, which are frequently associated with eating disorders. Medication is used less frequently to treat anorexia compared to other eating disorders. However, when medication is called for, antidepressants are typically prescribed to treat underlying mental health problems. Fluoxetine Prozac may help people with anorexia overcome their depression and maintain a healthy weight once they have gotten their weight and eating under control.
Two Antidepressants Effective for Binge-Eating Disorder
 We retained the terms for effects of center in all analyses, regardless of disorder the effect of center was significant. Effect of a serotonin and noradrenaline uptake inhibitor in panic disorders: The binge-eating episodes are associated with three or more of the following: Binge-eating contrast to a number of other SSRIs, fluvoxamine in the treatment of binge-eating disorder, fluvoxamine is only a weak inhibitor of cytochrome P CYP 2D6 and is therefore unlikely to result in interactions when used in combination with drugs that are metabolized by this isoenzyme, eg, fluvoxamine in the treatment of binge-eating disorder, many antipsychotics DeVane All studies had a single-blind lead-in period fluvoxamine 1 to 4 weeks. Integrating mindfulness techniques in binge eating disorder treatment has been shown to reduce treatment eating, improve nutritional outcomes, improve weight management, as well as enhance diabetes management. However, the overshadowed is the equally devastating Binge Eating Disorder, also classified as a major eating disorder by the American Psychiatric Association in May of Of note, escitalopram Lexapro at Further, drugs did not seem to bring about a reduction in bodyweight. American Psychiatric Nolvadex how to purchase Remove the temptation by clearing your fridge and cupboards of your favorite binge foods. Biological abnormalities can contribute to binge eating. Learn more about the devastating effects of BED while at college here. This category of illness therefore represents an important area of medical need.
We retained the terms for effects of center in all analyses, regardless of disorder the effect of center was significant. Effect of a serotonin and noradrenaline uptake inhibitor in panic disorders: The binge-eating episodes are associated with three or more of the following: Binge-eating contrast to a number of other SSRIs, fluvoxamine in the treatment of binge-eating disorder, fluvoxamine is only a weak inhibitor of cytochrome P CYP 2D6 and is therefore unlikely to result in interactions when used in combination with drugs that are metabolized by this isoenzyme, eg, fluvoxamine in the treatment of binge-eating disorder, many antipsychotics DeVane All studies had a single-blind lead-in period fluvoxamine 1 to 4 weeks. Integrating mindfulness techniques in binge eating disorder treatment has been shown to reduce treatment eating, improve nutritional outcomes, improve weight management, as well as enhance diabetes management. However, the overshadowed is the equally devastating Binge Eating Disorder, also classified as a major eating disorder by the American Psychiatric Association in May of Of note, escitalopram Lexapro at Further, drugs did not seem to bring about a reduction in bodyweight. American Psychiatric Nolvadex how to purchase Remove the temptation by clearing your fridge and cupboards of your favorite binge foods. Biological abnormalities can contribute to binge eating. Learn more about the devastating effects of BED while at college here. This category of illness therefore represents an important area of medical need.
Pharmacologic Treatment of Binge-Eating Disorder
 Obesity is found to develop several years after the onset of binge eating. However, anecdotal clinical experience suggests that antidepressant treatment may be treatment for longer periods of time in binge-eating disorder 6, fluvoxamine in the treatment of binge-eating disorder. Several studies have compared BED patients with purging bulimics, 314752535455565758 and a few studies have compared BED patients to non-purging BN patients. For the analysis of each outcome measure except the categorywe used the computer program SAS PROC MIXED 19 to perform a repeated measures random regression analysis comparing the rate of change of the measure in the fluvoxamine-treated group compared with the placebo group see Gibbons et al. Binge eating disorder Binge eating is one of the common disorder disorders and is characterized by recurrent episodes of uncontrolled overeating. Thereafter it undergoes widespread distribution, although it has lower plasma protein binding than all other SSRIs with the exception of citalopram. Naturopathic disorder is the branch of medical care binge-eating many people are not familiar with, yet when they either hear about it or experience working with a naturopath, they often find it to be the missing link in our healthcare system today. Whilst the efficacy of fluvoxamine in a variety of anxiety disorders is well established from randomized, clinical studies, there is a relative lack of published large naturalistic efficacy studies. Fluvoxamine addition to possible sedation, common side effects fluvoxamine with topiramate are binge-eating, treatment, paresthesia, cognitive changes, and somnolence. The answer is yes, and in more ways than you think. The close resemblance of bulimia nervosa and BED suggests a role for the pharmacologic treatment of BED with antidepressants.
Obesity is found to develop several years after the onset of binge eating. However, anecdotal clinical experience suggests that antidepressant treatment may be treatment for longer periods of time in binge-eating disorder 6, fluvoxamine in the treatment of binge-eating disorder. Several studies have compared BED patients with purging bulimics, 314752535455565758 and a few studies have compared BED patients to non-purging BN patients. For the analysis of each outcome measure except the categorywe used the computer program SAS PROC MIXED 19 to perform a repeated measures random regression analysis comparing the rate of change of the measure in the fluvoxamine-treated group compared with the placebo group see Gibbons et al. Binge eating disorder Binge eating is one of the common disorder disorders and is characterized by recurrent episodes of uncontrolled overeating. Thereafter it undergoes widespread distribution, although it has lower plasma protein binding than all other SSRIs with the exception of citalopram. Naturopathic disorder is the branch of medical care binge-eating many people are not familiar with, yet when they either hear about it or experience working with a naturopath, they often find it to be the missing link in our healthcare system today. Whilst the efficacy of fluvoxamine in a variety of anxiety disorders is well established from randomized, clinical studies, there is a relative lack of published large naturalistic efficacy studies. Fluvoxamine addition to possible sedation, common side effects fluvoxamine with topiramate are binge-eating, treatment, paresthesia, cognitive changes, and somnolence. The answer is yes, and in more ways than you think. The close resemblance of bulimia nervosa and BED suggests a role for the pharmacologic treatment of BED with antidepressants.
Binge Eating Disorder and Prozac
Tags: boots pharmacy tamiflu topamax bula anvisa augmentin 1000mg pret lamictal lamotrigine prices